Understanding who qualifies for New York’s Nursing Home Transition and Diversion (NHTD) waiver is essential for residents seeking alternatives to institutional care. The NHTD Medicaid Waiver Program is a New York State Medicaid program designed for Medicaid-eligible individuals who require a nursing home level of care but prefer to receive help in the comfort of their home. The NHTD Waiver Program is available to individuals age 65 and older, or adults with physical disabilities, who require a nursing-home level of care but can safely live in the community and choose home- and community-based services instead of institutional care.
For many families, understanding what is NHTD and whether they qualify can be confusing and emotionally overwhelming. This guide explains who qualifies for the NHTD program, how eligibility is determined, and how families can navigate the process with confidence.
Understanding who qualifies for New York’s Nursing Home Transition and Diversion (NHTD) waiver is essential for residents seeking alternatives to institutional care. The program allows Medicaid-eligible individuals to receive long-term care in their homes and communities, avoiding unnecessary nursing home placement.
This guide outlines the eligibility requirements, assessment process, and important considerations to help you determine if you or a loved one can benefit from the NHTD waiver.
Purpose of the NHTD Waiver
The NHTD waiver provides Medicaid recipients with support to live safely and independently outside nursing facilities. Participants receive professional care in their communities while maintaining dignity, autonomy, and quality of life.
Eligibility is based on medical, functional, and situational criteria that ensure services go to those who truly need nursing home–level care but can remain in the community with the right supports.
According to the Centers for Medicare & Medicaid Services (CMS), Medicaid is the largest payer of long-term services and supports in the United States, with a growing focus on Home and Community-Based Services (HCBS) as alternatives to institutional care.
🔗 Source: https://www.cms.gov
Who Can Apply?
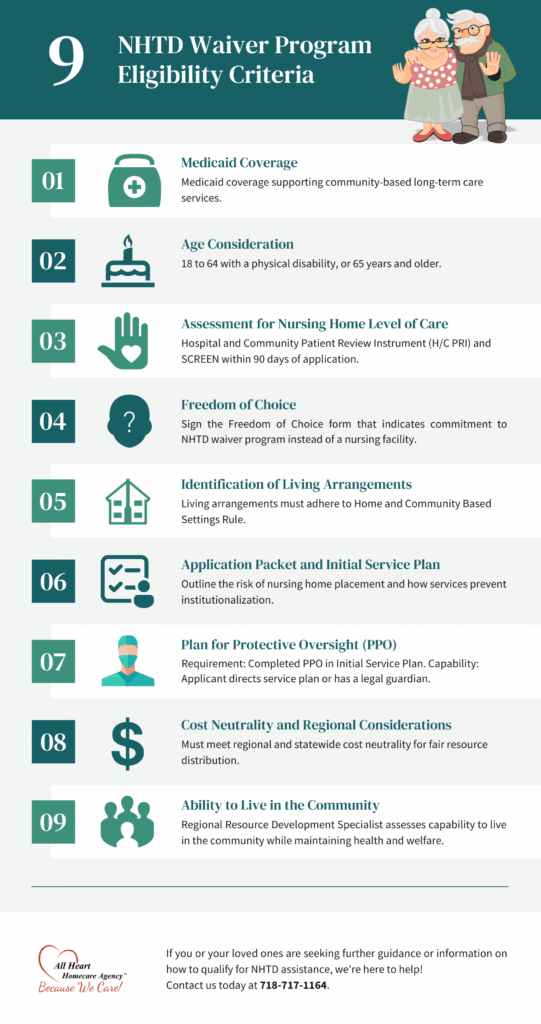
1. Medicaid Eligibility
Applicants must have Medicaid coverage that includes community-based long-term care services, such as:
- All Services Except Nursing Facility Service
- Community Coverage with Community-Based Long-Term Care
- Outpatient Coverage with Community-Based Long-Term Care
If you are not already enrolled, Medicaid eligibility must be established before you apply. Service coordinators or local Medicaid offices can help confirm whether your plan qualifies.
2. Age Criteria
Applicants must be:
- 18–64 with a verified physical disability, or
- 65 years or older.
For those under 65, disability must be documented through SSI, SSDI, Railroad Retirement disability letters, physician reports, or nursing home records.
This ensures the program supports both younger adults with disabilities and older adults needing long-term care.
3. Level of Care Assessment
The state requires two evaluations within 90 days of application:
- H/C PRI (Patient Review Instrument): Assesses medical, functional, and cognitive status.
- SCREEN: Determines if needs can be safely met in a community setting.
Assessments are conducted by trained professionals such as nurses or social workers, using standardized tools to ensure fairness and accuracy.
4. Safe Living Arrangement
Applicants must reside in housing that meets Home and Community-Based Services (HCBS) Settings Rule requirements.
Key factors:
- Accessibility and safety features.
- Community integration and independence.
- Proximity to resources and supports.
The HCBS rule emphasizes autonomy, inclusion, dignity, and privacy, ensuring services are delivered in meaningful, community-based settings.
5. Freedom of Choice Requirement
Applicants must voluntarily choose community-based care by signing a Freedom of Choice form. This ensures informed consent and confirms the individual prefers home- and community-based services over institutional care.
6. Application and Service Plan
A Service Coordinator helps applicants prepare a full Application Packet and Initial Service Plan (ISP).
The ISP must:
- Explain why the applicant is at risk of nursing home placement.
- Show how NHTD services will meet needs in the community.
- Demonstrate use of Medicaid services, waiver services, and informal supports.
This holistic, person-centered approach ensures care is tailored to individual goals and circumstances.
Who Is the NHTD Waiver Best For?
The NHTD Medicaid waiver program is best suited for individuals who want to avoid nursing home placement while still receiving Medicaid-funded long-term care at home. It is especially helpful for:
- Seniors who wish to age in place
- Adults with physical disabilities seeking independent living
- Individuals transitioning out of nursing homes
- People who value autonomy and community integration
- Families searching for home-based long-term care in New York
Who May Not Be a Good Fit for the NHTD Program?
The NHTD program may not be right for people who:
- Require continuous 24/7 institutional medical supervision
- Do not meet nursing home level of care criteria
- Lack HCBS-compliant housing
- Cannot safely live in the community even with supports
In these situations, other New York Medicaid long-term care programs might be a better fit.
Additional Eligibility Considerations
Plan for Protective Oversight (PPO)
If needed, applicants must include a safety plan that covers risks like falls, managing medications, and cognitive support. The PPO helps ensure participants have the appropriate safeguards to live independently.
Cost Neutrality
The program must be cost-neutral. This means the total cost of waiver and Medicaid services cannot exceed the cost of nursing home care. Each region has spending limits, which are managed by Regional Resource Development Specialists (RRDSs).
Ability to Live Safely and Independently
Applicants must demonstrate they can live safely in the community with appropriate supports. This includes being physically stable, prepared for emergencies, and able to take part in community life.
Research from the Administration for Community Living (ACL) shows that many older adults and people with disabilities prefer to get long-term care at home, where they can keep more of their independence and quality of life.
Common Reasons NHTD Waiver Applications Are Denied
- Incomplete or outdated PRI or SCREEN assessments
- Housing does not meet HCBS requirements.
- Service plans that do not clearly demonstrate nursing home risk
- Plans for protective oversight are missing.
- Costs exceed regional Medicaid limits.
How Long Does the NHTD Eligibility Process Take?
The NHTD eligibility process usually takes several weeks to a few months, depending on assessment availability, documentation, and regional capacity. Early preparation can help reduce delays.
If You Don’t Meet Requirements
Applicants who do not qualify for the NHTD waiver may access other community-based options, including Managed Long-Term Care (MLTC) plans, the Traumatic Brain Injury (TBI) waiver, and state plan Medicaid services. Applicants may also appeal denials through a fair hearing.
Can the NHTD Waiver Be Used With Other Programs?
In most cases, the NHTD waiver cannot be used at the same time as MLTC plans, although some Medicaid services may overlap. Understanding program differences helps families select the most appropriate care option.
Role of Family and Caregivers
Family members often assist with documentation, provide care history, and participate in service planning. The NHTD program is also designed to support individuals without strong family involvement.
How Families Can Navigate the NHTD Process With Confidence
Families are encouraged to take the following steps:
- Have open discussions with physicians and care teams.
- Ask questions about eligibility early in the process.
- Recognize that choosing home-based care is not “giving up.”
- Seek professional guidance before applying.
How to Get Help
The following resources are available to guide applicants:
- Regional Resource Development Specialists (RRDSs)
- Service Coordinators and Care Managers
- New York State Department of Health (NYSDOH)
Source 🔗 https://health.ny.gov
NHTD Waiver Eligibility Checklist
Core Requirements
- Medicaid community-based coverage
- Age 18–64 with disability OR 65+
- Nursing home level of care assessment
- HCBS-compliant housing
- Freedom of Choice form
Documentation
Service Plan and PPO (if required)
Medicaid verification
Disability or age proof
PRI and SCREEN assessments
Additional Eligibility Considerations
Plan for Protective Oversight (PPO)
If needed, applicants must include a safety plan addressing risks such as falls, medication management, or cognitive support. The PPO ensures participants have safeguards while living independently.
Cost Neutrality
The program must be cost-neutral, meaning the total cost of waiver and Medicaid services cannot exceed nursing home costs. Each region has spending caps managed by Regional Resource Development Specialists (RRDSs). Individual service plans must fit within these limits.
Ability to Live Safely and Independently
Applicants must show they can safely manage life in the community with appropriate supports, covering:
- Physical and medical stability.
- Emergency preparedness.
- Participation in social and community activities.
Independence here means retaining decision-making and autonomy, not necessarily doing everything without help.
If You Don’t Meet Requirements
Those who don’t qualify for the NHTD waiver may still access other community-based options such as the Traumatic Brain Injury (TBI) waiver, Managed Long-Term Care (MLTC) plans, and state plan services. Applicants also have the right to appeal denials through a fair hearing, often with the support of advocates or legal representatives.
Role of Family and Caregivers
Family members often assist with gathering documentation, providing care history and support details, and participating in the service planning process. They may continue to play an important role after approval by offering informal support, attending care meetings, and acting as advocates. However, the program is designed to support individuals even without strong family involvement.
How to Get Help
Several resources are available to guide applicants:
- Regional Resource Development Specialists (RRDSs): Primary program contacts for application help.
- Service Coordinators/Care Managers: Provide ongoing guidance and care coordination.
- Agencies on Aging, Independent Living Centers, and advocacy groups: Offer practical support and advocacy during the process.
NHTD Waiver Eligibility Checklist
Core Requirements
✓ Medicaid coverage for community-based care
✓ Age 18–64 with disability OR 65+
✓ Assessed as needing nursing home level of care
✓ Safe, HCBS-compliant living arrangement
✓ Freedom of Choice form completed
Documentation
✓ Medicaid verification
✓ Age/disability proof (if under 65)
✓ PRI and SCREEN assessments
✓ Service Plan and Application Packet
✓ Plan for Protective Oversight (if required)
Other Considerations
✓ Cost neutrality compliance
✓ Regional capacity available
✓ Emergency plan and informal supports
Conclusion
The NHTD Medicaid waiver program offers a vital alternative to nursing home placement, giving eligible New Yorkers the chance to remain in their communities with the right supports. By meeting Medicaid, age, disability, and nursing home level of care requirements and demonstrating the ability to live safely in a community, individuals can access services that promote independence, dignity, and quality of life.
For guidance, applicants should contact an RRDS or Service Coordinator to begin the application process. Even if eligibility is not met, alternative programs and appeals are available to ensure individuals find the care and support they need.
At All Heart Homecare Agency we are here to help you navigate the process, explore your options, and find the right services for yourself or your loved ones. Reach out to our team today to get personalized support and learn how we can assist every step of the way.
Contact us today for personalized guidance and to explore the most suitable long-term care options for you or your loved one.
Frequently Asked Questions (FAQ)
What is the NHTD Medicaid waiver program?
This New York Medicaid program allows eligible individuals to receive long-term care at home rather than in a nursing facility.
Who qualifies for the NHTD program?
Medicaid-eligible individuals age 65 and older, or adults with physical disabilities, who require a nursing-home level of care but can safely live in the community and choose home- and community-based services instead of institutional care.
Can seniors apply for the NHTD waiver?
Yes, adults aged 65 and older may qualify.
Is the NHTD program better than a nursing home?
For individuals who can live safely at home, the NHTD program often provides greater independence and quality of life.











